Understanding Neuropathy and Why It Hurts
Neuropathy (often called peripheral neuropathy) happens when nerves that carry messages between the brain, spinal cord, and the rest of the body become damaged or irritated. These nerves can misfire, sending pain signals even when there’s no immediate injury. That’s why neuropathy pain can feel confusing and unpredictable—burning, tingling, stabbing, electric “zaps,” numbness, or extreme sensitivity to touch.
Neuropathy has many possible causes, including diabetes, vitamin deficiencies (like B12), autoimmune conditions, chemotherapy, infections, alcohol use, thyroid issues, and nerve compression. Pain management works best when it combines symptom relief with a plan to address the underlying cause whenever possible.
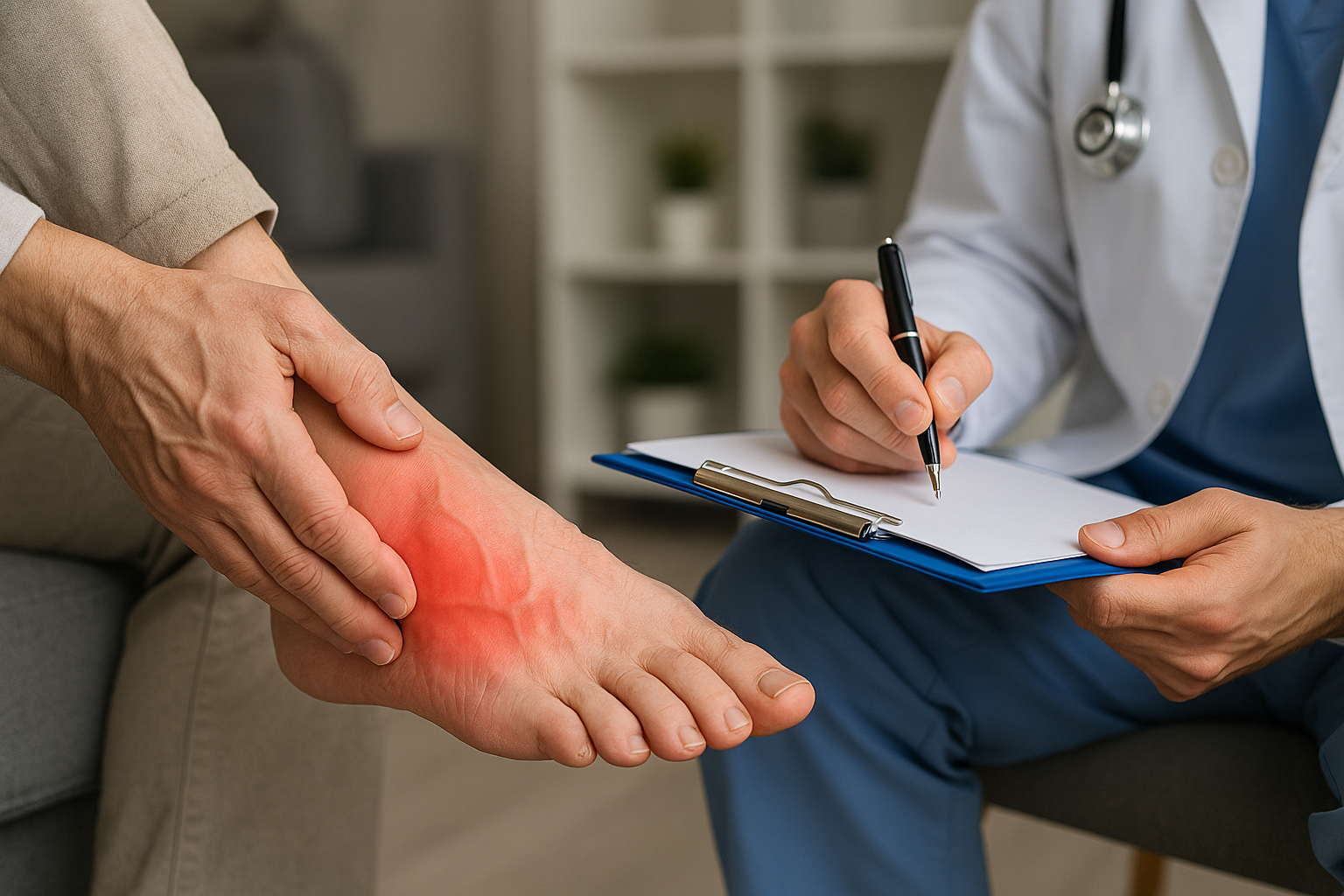
Common Symptoms and When to Seek Help
Neuropathy symptoms vary, but many people notice them first in the feet or hands. Symptoms may be mild at first and gradually become more intense. Paying attention early can make treatment more effective.
Symptoms that often respond well to a treatment plan
- Burning, tingling, or “pins and needles” sensations
- Numbness or reduced ability to feel temperature or pain
- Shooting or stabbing pain, especially at night
- Hypersensitivity (even light touch can hurt)
- Muscle weakness, cramping, or balance issues
When to get medical care urgently
- Sudden or rapidly worsening weakness
- New numbness after an injury or fall
- Loss of bladder or bowel control
- Severe pain with swelling, redness, fever, or a new rash
- Foot wounds that aren’t healing, especially with diabetes
If your symptoms are new, changing quickly, or affecting your daily function, a clinician can help identify the cause and recommend targeted neuropathy pain management strategies.
Neuropathy Pain Management: Treatments That Can Help
Because neuropathy pain is nerve-based, it often doesn’t respond well to typical pain relievers alone. The most effective approach is usually layered: medications, physical strategies, lifestyle changes, and careful prevention of flare-ups.
Medications commonly used for nerve pain
Medication choices depend on your health history, the suspected cause, and how the pain presents. Many people do best with gradual dose changes and consistent follow-up to balance relief with side effects.
- Anticonvulsants (often used for nerve pain): options like gabapentin or pregabalin may reduce “misfiring” nerve signals.
- Antidepressants (also used for pain): certain SNRIs or tricyclic antidepressants can help calm pain pathways and improve sleep.
- Topical treatments: lidocaine patches or capsaicin creams may help localized burning or sensitivity with fewer whole-body side effects.
- Carefully selected pain relievers: NSAIDs may help if inflammation or a musculoskeletal issue is also present, but they’re often limited for pure neuropathic pain.
- Opioids: sometimes considered for short-term or severe cases, but generally not first-line due to risks and limited long-term benefit for neuropathic pain.
Tip: If a medication helps but causes drowsiness, dizziness, or swelling, ask about timing, dosage adjustments, or alternatives rather than stopping abruptly.
Physical therapy and movement-based strategies
Gentle, consistent movement supports circulation, reduces stiffness, and may improve balance and confidence—especially when neuropathy affects the feet. A physical therapist can tailor a plan to your symptoms and fall risk.
- Balance and gait training to reduce falls
- Strengthening for ankles, legs, hips, and core
- Nerve gliding exercises when appropriate (especially with nerve compression patterns)
- Low-impact cardio like walking, cycling, or water exercise to support circulation and blood sugar control
Start small and build gradually. Overdoing activity can trigger symptom flares in some people, so a paced approach often works best.
Lifestyle changes that reduce neuropathy flare-ups
Lifestyle changes won’t replace medical care, but they can significantly improve day-to-day comfort and slow progression—particularly for diabetic neuropathy or metabolic causes.
- Blood sugar management: steady glucose levels are one of the most powerful tools for diabetic neuropathy pain management.
- Sleep support: neuropathy pain often worsens at night. A consistent schedule, a cool room, and avoiding late caffeine can help.
- Limit alcohol: alcohol can worsen nerve damage and interfere with sleep quality.
- Quit smoking: nicotine reduces blood flow to nerves and can intensify symptoms.
- Nutrition for nerve health: adequate protein and nutrients, and checking for deficiencies (especially vitamin B12) when recommended.
Small changes add up. Many people find that improving sleep and stabilizing blood sugar reduces how “loud” the nerve pain feels.
Complementary therapies and at-home relief
Many people use complementary approaches alongside medical treatment. The goal is comfort, better function, and fewer flare-ups.
- Heat or cold therapy: some prefer warmth for stiffness; others find brief cold packs reduce burning. Avoid extremes if you have numbness to prevent skin injury.
- Massage: may help with muscle tension and circulation; communicate clearly about pressure if touch sensitivity is an issue.
- Acupuncture: some people report improvements in pain and sleep.
- TENS unit: mild electrical stimulation may reduce pain signals for certain individuals.
- Mind-body strategies: breathing exercises, meditation, and gentle yoga can help reduce stress-driven pain amplification.
Track your symptoms for a couple of weeks when trying something new. A simple note like “pain level, sleep quality, activity, and triggers” can reveal patterns and help you make smarter adjustments.
Protecting Your Feet and Preventing Complications
If neuropathy affects your feet, prevention becomes a key part of pain management. Numbness can make it harder to notice blisters, cuts, or pressure points, which can lead to infections and slow healing.
Daily habits that make a big difference
- Check your feet daily for redness, cracks, blisters, or sores (use a mirror for the soles).
- Choose supportive footwear with a wide toe box and cushioned soles; avoid tight shoes that create pressure points.
- Keep skin moisturized (but avoid lotion between toes, where moisture can increase fungal risk).
- Trim nails carefully or consider podiatry support if vision or flexibility is limited.
- Protect from temperature extremes—test bath water with your hand or a thermometer if your feet are numb.
If you have diabetes or circulation concerns, regular foot exams can catch problems early and help you stay active with less pain.
Creating a Personalized Neuropathy Pain Management Plan
Neuropathy pain is personal—what works well for one person may not work for another. A strong plan usually includes (1) confirming or addressing the cause, (2) reducing pain and improving sleep, and (3) building safer movement and daily routines.
Questions to discuss with your healthcare provider
- What is the most likely cause of my neuropathy, and what tests are appropriate?
- Which medication options fit my health history and other prescriptions?
- What side effects should I watch for, and when should I follow up?
- Would physical therapy, podiatry, or a pain specialist help?
- What are realistic goals for pain reduction and function over the next 4–12 weeks?
Progress may be gradual, but many people do see meaningful improvements—especially when pain relief, lifestyle support, and prevention work together.
Conclusion
Neuropathy pain management is most effective when it’s comprehensive: treating nerve pain with the right therapies, addressing root causes, and protecting your daily function—especially foot health and balance. With a personalized plan and consistent follow-up, it’s possible to reduce symptoms, improve sleep, and regain confidence in everyday activities.